Episode #184 Keeping Patients Safe from Unavoidable Human Error
January 10, 2024Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
Our featured article today is from the October 2023 APSF Newsletter. It is, “Achieving a Successful Patient Safety Program with Implementation of a Harm Reduction Strategy” by Jonathan Cohen. Thank you to Jonathan Cohen for contributing clips to the show today.
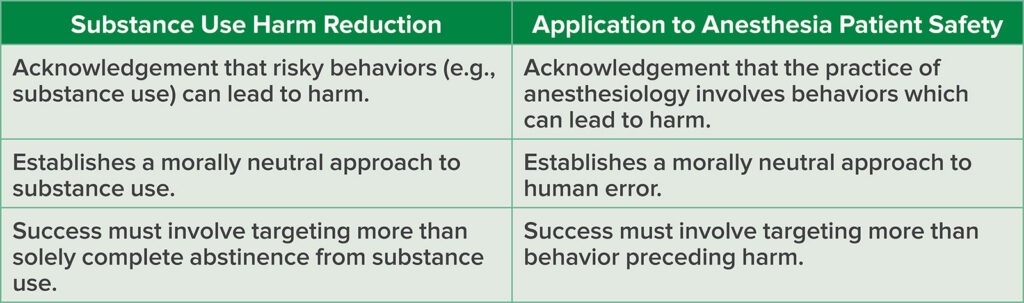
Check out Table 1 in the article which provides substance use harm reduction strategies that may be applied to harm reduction for anesthesia patient safety.
Table 1: Analogy of Harm Reduction Approach with Substance Use and Anesthesia Patient Safety.
Here are three principles described in the article to help keep patients safe with a harm reduction approach in anesthesiology.
- Acknowledgement that the practice of anesthesiology involves behavior that can lead to harm.
- Establishment of a morally neutral approach to human error.
- Achievement of success by targeting more than the behavior preceding harm.
Subscribe to our YouTube Channel here: https://www.youtube.com/@AnesthesiaPatientSafety
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2024, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. It is almost time for the February 2024 APSF Newsletter, but we still have some great articles from the October 2023 Newsletter to review. Today, we are talking about how to keep patients safe during anesthesia care provided by anesthesia professionals who are human and thus prone to human error.
Before we dive into the episode today, we’d like to recognize Blink Device Company, a major corporate supporter of APSF. Blink Device Company has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Blink Device Company – we wouldn’t be able to do all that we do without you!”
Our featured article today is from the October 2023 APSF Newsletter. It is, “Achieving a Successful Patient Safety Program with Implementation of a Harm Reduction Strategy” by Jonathan Cohen. To follow along with us, head over to APSF.org and click on the Newsletter heading. First one down is the Current Issue. Then, scroll down until you get to our featured article today. I will include the link in the show notes as well.
Before we get into the article, we are going to meet the author. Let’s take a listen.
[Cohen] “Hi, my name is Jonathan Cohen and I’m an anesthesiologist at Moffitt Cancer Center in Tampa, Florida.”
[Bechtel] To kick off the show today, I asked Cohen why he wrote this article. This is what he had to say.
[Cohen] “We can learn a lot about how to manage challenging patient safety issues from fields outside of medicine, including economics, psychology, business, and in this case, public health. The concept of harm reduction emerged decades ago with its focus on decreasing the negative consequences of behaviors rather than attempts to solely eliminate them.
Making errors is something that all humans have the capacity for. Aviation psychologist Scott Chappelle and Douglas Wegman stated human beings by their very nature make mistakes. Therefore, it is unreasonable to expect error free human performance. From the harm reduction perspective, we can learn to stop treating errors as moral failures and blaming the anesthesia professionals making them.”
[Bechtel] Thank you so much to Cohen for helping to introduce this important concept of harm reduction. And now it’s time to get into the article. Cohen opens with a recent example of a “harm reduction” approach and some definitions. First up, “Prevalence reduction” approach depends on abstinence from behaviors that create risk. “Harm reduction” approach on the other hand relies on modifying the harmful consequences of the behavior and this is especially beneficial when the behavior is difficult to modify such as with substance use and abuse. The example is from March 2023 when the US Food and Drug Administration approved naloxone hydrochloride nasal spray for over the counter, nonprescription use to help reduce harm associated with opioid use, overuse, or abuse. This approach has long been recommended by the American Society of Anesthesiologists. Keep in mind that harm reduction approaches may be opposed by people who are morally opposed to the behavior. Other examples of harm reduction include using prescribing cholesterol-lowering and antihyperglycemic medications for patients without optimal diet and exercise behaviors.
Check out Table 1 in the article which provides substance use harm reduction strategies that may be applied to harm reduction for anesthesia patient safety. Don’t worry I will include this table in the show notes as well. The first row refers to the acknowledgement that the risky behavior of substance use can lead to harm which is similar to the acknowledgement that the practice of anesthesiology involves behaviors that can lead to harm. The second row reveals that harm reduction establishes a morally neutral approach to substance use and this may be applied to anesthesia patient safety by establishing a morally neutral approach to human error. The third row describes success with the harm reduction approach that must involve targeting more than solely complete abstinence from substance use. Similarly, anesthesia patient safety success must involve targeting more than behaviors preceding harm.
Now, let’s look a little closer at what a harm reduction approach applied to anesthesia patient safety looks like. First up, we must acknowledge that the practice of anesthesiology involves behavior which can lead to harm. Providing anesthesia care is complex, time-constrained, and stressful and requires interacting with the patient, equipment, environment, medications, tasks, organizations, and the surgical team. Anesthesia professionals are called upon to remain vigilant at all times, be able to multi-task or rapidly task switch between several tasks and take actions that may have life or death consequences. For all of these reasons, it is easy to see that the practice of anesthesiology can lead to harm. The key to successful and safe anesthesia practice is significant practice to be able to manage all of these factors, tasks, and relationships while also being prepared for unplanned events. Anesthesia professionals are often compared to pilots and studies have shown that for experienced pilots, complex task management combined with integrating unplanned tasks and rescheduling tasks does not require significant mental effort and the same is true with experienced anesthesia professionals. On the other hand, novice anesthesia professionals report an increased subjective workload for a given task load compared to experienced anesthesia professionals. It is important to consider that even as we work towards a goal of no patient harmed by anesthesia care, there is an inherent risk of the anesthesia care, the surgical procedure, and the patient comorbidities. This risk ranges from serious patient harm, which is rare, to near misses. We must also consider that when harm occurs to patients due to an error, this can have lasting effects on the anesthesia professional as well.
So, where do we go from here? The next step is to make errors morally neutral. This is important if we believe Shappell and Wiegmann who tell us that it is unreasonable to expect error-free performance from humans because humans, by their very nature, make mistakes. The literature confirms this as well. A study by Perrow estimated that human error is responsible for 60-80% of accidents. This is similar to the anesthesia-specific findings by Cooper and colleagues from their study, “Preventable anesthesia mishaps: a study of human factors” published in 1978 which reported that about 80% of the preventable incidents were due to human error and included breathing circuit disconnections, inadvertent changes in gas flow, and drug0syringe errors being the most common problems.
So, what does normal human error look like? We may make 5-20 errors each hour depending on the type of work, either manual compared to cognitive, and the circumstances if the work is routine or urgent. Now, this may be a significant number of errors, but harm is prevented by the systems in which we work. Flexible and resilient systems have appropriate barriers, recoveries, and redundancies to prevent errors from causing harm. Harm may occur when the adaptive capacity of the system cannot be maintained. This may be the case depending on factors related to the anesthesia professional including fatigue, distraction, or misinterpretation of clinical data or a warning alarm combined with certain patient factors including significant comorbidities and decreased physiologic reserve and certain surgical procedure factors including complexity of the procedure, communication, equipment, and environment.
When medical errors occur, there is a tendency to see it as a moral failing and place blame on the individual for not paying attention or acting in a way that was only obviously wrong to those viewing the situation in hindsight. We have learned that this blame approach does not improve performance or decrease error rates. Instead, it makes it harder to report errors and learn from these events. Unfortunately, blame for making errors is still quite common. We really need to move on to creating and maintaining a “Just Culture.” One of the fundamentals of a “Just Culture” is to move away from punitive language and acknowledge that behavior can be seen as the cause of errors even if the behavior it not attributed to impropriety or intentions of harm. Another important consideration is that there is still accountability in a Just Culture, but it is balanced between the individual and the system within which the individual practices. Cohen tells us that it is possible to hold individuals accountable without blame. We can see this in the model for substance abuse.
The future of safer anesthesia care depends on abandoning the elimination of error-prone behavior approach. Indeed, human factors experts report that it will not work. The traditional Safety-I approach was to examine what went wrong. Going forward, we need to move on to the Safety-II approach which evaluates what is necessary for acceptable and satisfactory outcomes to occur given known human performance variability constraints. You can think of this approach as proactive safety management instead of the reactive blame approach of Safety-I. The Safety-II approach relies on paying attention to the system that shapes the variability in human performance. Modifications to the system to decrease harm are more likely to be long-lasting and effective when compared to interventions aimed at modifying individual behaviors.
What does a harm reduction practice look like in anesthesiology? Let’s take a look at Table2 in the article for an example of Harm reduction related to wrong-sided nerve block.
- The first harm reduction principle is to acknowledge that the practice of anesthesiology involves behavior that can lead to harm. The goal is to reduce the risk of harm from errors to both patients and anesthesia professionals. The tactics include developing a robust safety program to manage risk of harm to patients, including providing care for the patient/family as well as the anesthesia professional. The example here is after a wrong-sided nerve block, the patient was immediately cared for and the event was promptly reviewed and disclosed to the patient and family. Support was provided to the anesthesia professional as well.
- The next harm reduction principle includes establishing a morally neutral approach to human error. The goal is for health care to adopt the notion that error is ubiquitous, unavoidable, and therefore not blameworthy. The tactics are establishment of a just culture, which supports reporting adverse events, which is a critical step towards reducing harm. In the example, the anesthesia professional understood that by reporting the events, systemic issues that contributed to the error occurring could be reduced.
- The third harm reduction principle is that success must involve targeting more than the behavior preceding harm. The goal is to focus on preventing harm from error. The tactics include targeting systems-level solutions that create barriers to prevent errors, recoveries to capture error, and redundancies to limit the effects of error when it occurs. Returning to our example, as a result of the wrong-sided nerve block, nerve block time outs were created that verified the procedure using multiple sources of information immediately prior to the block (including the patient when possible) and identified the site with a visible mark prior to performance of the procedure.
As you can see this harm reduction approach is very different than just blaming the individual who performed the wrong sided nerve block and with this new approach the system has been modified to decrease the risk of harm in the future. Cohen reminds us that anesthesia professionals of all experience levels will make errors and then this happens, and it will happen, there should be no blame assigned to the individual and the error needs to be treated as morally neutral. There is a call to action to create a Just Culture to balance accountability between the individual and the system with a focus on designing systems that prevent harm rather than human error. The practice of anesthesiology must continue to adapt and grow with additional safety training and collaborations with safety professionals to understand and improve our complex systems.
[Bechtel] We made it to the end of the article, but before we wrap up for today, we are going to hear from Cohen once again. I also asked him what he hopes to see going forward. Here’s his response.
[Cohen] “Despite the popularization of a just culture approach in healthcare, blame for medical errors continues. This blame doesn’t just come from above on the hierarchy, but from colleagues as well. Attempts to eliminate error prone behavior have historically failed.
Applying the harm reduction approach to patient safety allows us to view errors for what they are, morally neutral events. By reducing the stigma of making errors, anesthesia professionals will be more likely to come forth with information that can help us build more robust safety systems, making errors less likely to occur, as well as reducing harm from them when they inevitably do occur.”
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
Have you made any resolutions for 2024? We hope that continuing to provide safe anesthesia care is at the top of the list. There are so many resources from the APSF that can help you with this goal. Check out the Patient Safety Resources over at apsf.org which include look alike drug vials, the anesthesia patient safety podcast, the APSF video library, news and updates, in the literature, the APSF technology initiative with courses on low flow anesthesia and quantitative neuromuscular monitoring, emergency manuals implementation collaborative, perioperative multi-center handoff collaborative, patient guides, the COVID resource center, patient guides, International resources, and helpful links.
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2024, The Anesthesia Patient Safety Foundation